It has long been standard for Michigan residents to wait up to a month for their benefits applications to be approved or denied. As in many states, different programs, whether Medicaid or food assistance, have different allowable processing times.
Now imagine you’re the person or family in crisis, waiting for an answer on your case. Michigan’s Genesee County not only imagined this scenario before the pandemic hit, they mapped out the journey, said Lena Selzer, Cofounder and Senior Director of nonprofit Civilla. During that process, county leaders within the Michigan Department of Health and Human Services reframed the problem and asked a radical question: Why can’t we get people a same-day response when they apply for benefits?“
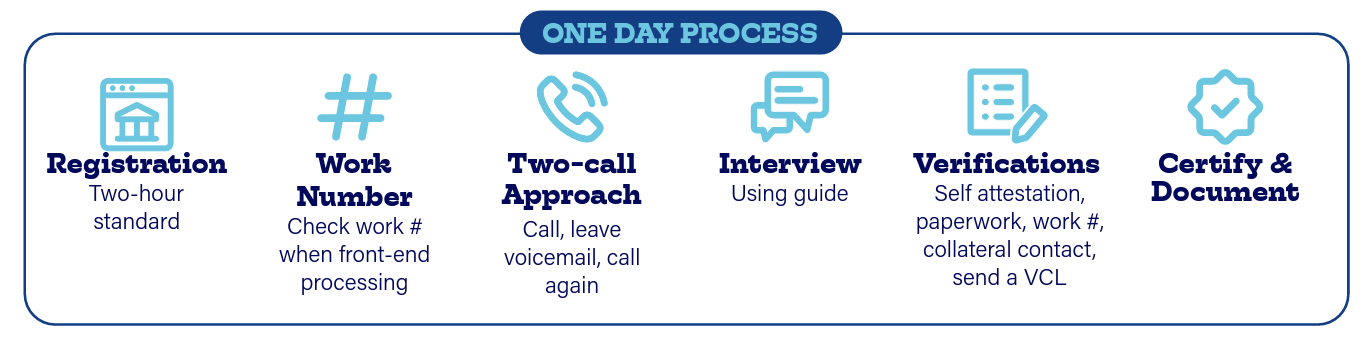
It was out of those conversations and contacts that the concept of One Day started to emerge, based on resident and staff needs,” said Sam Brennan, Design Lead at Civilla.
Reimagine and restructure policies
A key business process change that made the concept of One Day benefits delivery a reality was shifting the burden of collecting verification documents — such as pay stubs and lease agreements — from applicants to frontline staff, who are adept at gathering that information, Brennan said.
The process also uses self-attestation, or empowering applicants to verify or attest to certain things such as personal assets without providing additional documentation unless the information is questionable.
Rather than pause the One Day pilot, COVID-19 accelerated it from dozens of counties to launching statewide. As of September 2021 all health and human services offices statewide have been trained on the One Day process and are starting to implement the new model. Although every determination won’t happen in a day, that’s now the North Star guiding the process.
Some programs have policy and program limitations that won’t allow for single-day determinations. The goal is to build on best practices and expand One Day to Medicaid, child care, utility and cash assistance.
Reframe objectives
The One Day model was intuitive for staff, however there was a belief among some that having residents collect verification documents helped build self-sufficiency.
“It was a real mindset shift that [we] needed to have time and conversation around to say, ‘That’s actually not the vision,’” Brennan said. To help people reach success, they need basic support. Having them collect verifications doesn’t help them build self-sufficiency. Providing them with support quickly and efficiently does.
Codify best practices and expand
During the One Day pilot, frontline staff documented best practices for speeding up the verification process, including how-tos for framing requests for applicants and local office lists of common employers.
“In the pilot, we would hear about these efforts through interviews with staff. Together, we documented them and then shared them with others through trainings and communications,” Brennan said. “This sharing has continued through statewide rollout.” He added: “Create space to conduct a pilot prior to implementation and have a team focused on learning best practices as well as collecting and analyzing data. Next, during implementation, ensure that staff continue [to] have space to share what is working and not, so improvements can be documented and scaled.”





Leave a Reply
You must be logged in to post a comment.